MIT researchers have developed an implantable device that can automatically release glucagon when blood sugar levels drop dangerously low in Type 1 diabetes patients. The quarter-sized device contains a 3D-printed polymer reservoir that stores powdered glucagon and can be triggered wirelessly to deliver emergency doses. The study, led by Siddharth Krishnan and published in Nature Biomedical Engineering, demonstrates a potential solution for hypoglycemia episodes that occur during sleep or in patients who cannot recognize symptoms.
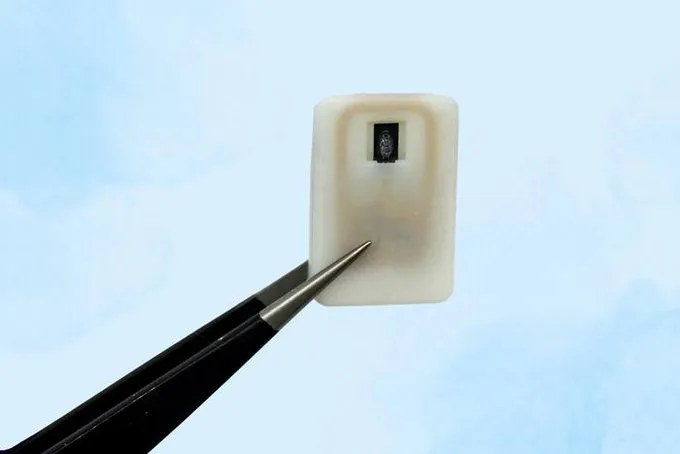
The device uses a nickel-titanium shape-memory alloy that changes from a flat slab to a U-shape when heated to 40 degrees Celsius. An antenna receives radiofrequency signals that trigger a small electrical current to heat the alloy, causing it to bend and release the drug contents. “This is a small, emergency-event device that can be placed under the skin, where it is ready to act if the patient’s blood sugar drops too low,” says Daniel Anderson, a professor in MIT’s Department of Chemical Engineering and senior author of the study.
In tests with diabetic mice, the device successfully reversed dropping blood sugar levels within 10 minutes of activation. The researchers also demonstrated the device’s ability to deliver epinephrine for treating heart attacks and severe allergic reactions. Blood sugar levels remained within normal ranges and prevented hypoglycemia during the study period.
The current version can store either one or four doses of glucagon and remained functional for up to four weeks in testing. The researchers plan to extend the device’s lifespan to at least one year and hope to begin clinical trials within three years. The device continued to work effectively even after fibrotic tissue formed around the implant, addressing a common challenge with implanted medical devices.
The research was funded by the Leona M. and Harry B. Helmsley Charitable Trust, the National Institutes of Health, a JDRF postdoctoral fellowship, and the National Institute of Biomedical Imaging and Bioengineering. The device could potentially interface with existing continuous glucose monitoring systems to provide automated emergency response for diabetes patients.
Source: news.mit.edu

